Although technology has made great strides, the patient experience and how people feel when using telehealth still has a lot of room for improvement.
A clunky interface or poor user experience can drive patients away, undermining trust, engagement, and even health outcomes. In fact, studies show that 90% of users abandon apps after a bad user experience.
Getting the patient experience right goes beyond making sure the video call technology works. It’s about making virtual care feel human. This means making patients feel comfortable, heard, and at ease from start to finish.
In this post, we’ll talk about how the design of telemedicine platforms can have a huge impact on how people experience their care and how product managers can improve that experience to keep patients engaged, comfortable, and satisfied.
Bad UX is killing retention and engagement in telehealth
Telemedicine offers a level of convenience that’s hard to beat. But many platforms still treat virtual visits as a digital version of in-person care, just with a video call instead of a face-to-face appointment. While that may sound good on paper, it overlooks a lot of important things that can make the experience feel personal and meaningful.
Simply having a functioning platform isn’t enough. If the user experience (UX) is poor, patients will drop off. Research shows that usability is one of the biggest reasons why people don’t stick with digital health tools. So, even though they log in for their first visit, if the experience is frustrating or confusing, they won’t come back.
Making a good first impression with onboarding
One of the first touchpoints for a patient is when they get onboarded to a platform. The process of joining a virtual call to talk to their clinician should feel seamless and intuitive. The reality, though, is that if the process is difficult or confusing, it can discourage patients from using the platform again.
For example, many video call platforms require users to jump through hoops like downloading an app and creating an account before they can attend a virtual consultation. This can be especially frustrating when combined with the stress of preparing for a medical appointment.
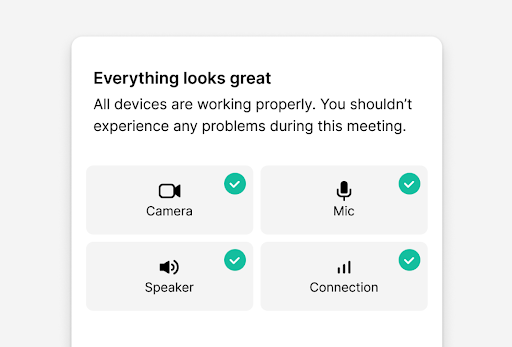
o make the best first iTmpression, telemedicine platforms should focus on simplifying the process. Having clear instructions, easy-to-follow steps, and even pre-call diagnostics that check device compatibility or internet connectivity can go a long way in reducing stress before the call even starts.
Creating comfort and building trust during calls
In healthcare, privacy and trust go hand in hand, and virtual care is no exception. While in-person visits naturally convey a sense of security, telehealth platforms must work harder to create that same level of confidence during a video call.
It’s up to healthcare providers and platform builders to make privacy and security a visible, reassuring part of the patient experience. That starts with choosing technology partners — such as video calling providers — who meet recognized compliance standards like HIPAA, GDPR, and ISO27001. These foundational choices help ensure that sensitive health information is protected from the moment a virtual visit begins.
But compliance alone isn’t enough. Patients need to see and feel that their data is being handled with care. Transparency is key: Clear communication around data use, recording, and sharing practices helps foster a sense of control and safety.
Design plays an important role here. Simple but thoughtful features like visible privacy indicators, real-time consent prompts, and straightforward language go a long way in building trust. When privacy is baked into both the backend and the user experience, patients are more likely to feel at ease, speak openly, and engage fully in their care.
Reducing mental fatigue for both patients and clinicians
It’s easy to overlook, but mental fatigue from video calls is a thing, especially if your clinicians have to sit in front of a screen for hours. A study from the University of Galway showed that the self-view on video calls led to mental fatigue.
Small design choices can make a huge difference here. How can the video layout support a natural flow of communication? Should the doctor’s video be larger, or should there be a space for eye contact? For example, giving patients the option to hide their self-view during the call can ease anxiety, and reduce fatigue or the distraction that it comes with.
Complex interfaces or too many clicks can also make the experience more draining than it needs to be. To minimize this, a design that keeps things simple and intuitive is important. Also, troubleshooting features, and keeping things like navigation clear and simple, go a long way in making consultations feel more comfortable.
Make accessibility a priority, not an afterthought
Telemedicine offers a solution for those with limited access to healthcare due to distance, mobility issues, or other barriers. However, accessibility goes beyond making sure patients can join the call. It’s also ensuring that everyone, regardless of their abilities or technical knowledge, can easily use the platform.
For example, choosing a video calling solution with features like closed captions, support for keyboard navigation or multi-language support can make telemedicine truly accessible for people who aren’t as comfortable with technology. It also applies to helping clinicians get accurate documentation with features like session transcriptions.
And it’s not just about meeting compliance standards; it’s about being a differentiator for telehealth platforms by creating a more inclusive experience. After all, you don’t want any patient to feel like they’re excluded from receiving care just because of their abilities or access to devices.
Keeping patients engaged after the session
Just because the video call ends doesn’t mean the work is done. Post-consultation is just as important as the call itself. If a patient logs off without clear next steps, they’re much less likely to stay engaged with their care.
A simple solution is to ensure that every consultation has a clear follow-up plan. Whether that’s automatic reminders, easy access to notes or prescriptions, or direct scheduling for a follow-up appointment, keeping patients in the loop after the call is crucial for long-term engagement.
Creating a more human virtual care experience
The goal of telemedicine should always be to provide high-quality, patient-centered care, no matter where the patient is located. That means focusing on design elements that make the experience not only easy to navigate but also comfortable, inclusive, and human-centered.
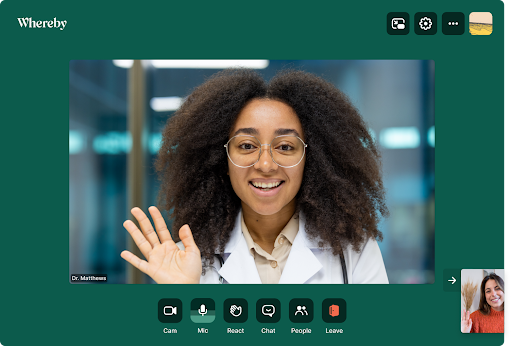
Choosing an intuitive video call provider like Whereby is a great start in prioritizing user experience. See how Whereby Embedded can improve your telemedicine platform with a smooth, secure, and easy-to-use video call API designed for telehealth.
Author: Niki Loboda, Business Development Director, Whereby