Key Takeaways:
- Telemedicine policy uncertainty impacts both patient access and clinician practice.
- Updated privacy and security regulations may address key patient and clinician concerns.
- Interstate licensure and unified guidelines are essential for sustained telemedicine growth.
Introduction
Administrative burdens and compliance challenges are among the biggest barriers to telemedicine adoption. Telemedicine growth has made navigating its complex regulatory landscape more critical than ever.
With the pandemic’s end, new legal challenges arose, demanding swift attention to maintaining telemedicine access and patient effectiveness. Here, we provide a concise overview of our regulation and compliance viewpoint, explain the current legal landscape governing telemedicine in the U.S., and present recommendations for improvement.
The Evolving Legal and Regulatory Landscape of Telemedicine
Post-pandemic policy changes began after the PHE ended on May 11, 2023. Lawmakers extended some waivers while debating long-term telemedicine policies. Since then, we have had a tumultuous 2024-2025 period in policy (see Figure 1).
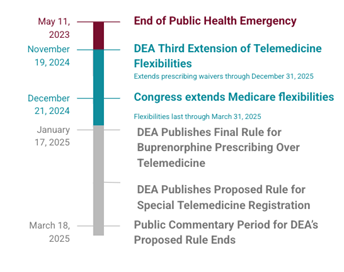
Figure 1. A brief overview of federal policy updates since the end of the PHE in 2023, including the DEA extending prescribing waivers, Congress working on extending Medicare flexibilities at the eleventh hour, and the DEA publishing their final and proposed rules in early January.
Along with these recent policy changes, clinicians must handle the underlying complexities of varying state regulations, licensure requirements, and reimbursement processes that directly affect how clinicians can successfully implement telemedicine from practice to practice. As healthcare regulations continue to change at the federal level, we anticipate facing unforeseen repercussions that could affect telemedicine, access for patients and clinicians, and healthcare disparities.
We consider key challenges and concerns we identified from legal and scientific literature surrounding telemedicine implementation and provide some recommendations and solutions as the US takes on the framework of telemedicine policy. Below, we explore three key issues that demand immediate attention.
Key Legal and Compliance Challenges in Telemedicine
Challenge 1: Privacy and Security Concerns
Health information security is a top concern for patients and clinicians using telemedicine. While all clinicians must use HIPAA-compliant telemedicine platforms since the end of the PHE, there are continued worries, such as patients unknowingly doing a telemedicine visit in a non-private space.
Additionally, with the release of many third-party applications–in mental health especially–there has been an increase in worry that HIPAA does not protect this data because patients do not share data directly with a clinician or organization. Concerns over patient health information security and privacy have led to states passing their own health data laws.
Challenge 2: Interstate Practice and Licensure
State-specific licensure requirements resurfaced after the PHE ended, complicating telemedicine practice across state lines. Although there are interstate licensure compacts, they do not all work in the same way as some are simply a platform to streamline obtaining all the needed licenses from states (Medical Licensure Compact for physicians) and others provide a single telemedicine license that works in all the participating states (Nurse Licensure Compact).
The streamlining of such compacts becomes more complex as each state must consider its own definitions of healthcare delivery, non-compete agreements, and standards of care. Clinicians consistently describe compliance concerns as a barrier to their using telemedicine. Such complaints apply to privacy and security and prescribing over telemedicine issues. These concerns imply that patients may lose access to healthcare when clinicians discontinue a convenient healthcare delivery option due to their compliance worries.
Challenge 3: Prescribing Over Telemedicine
Relevant to interstate practice as well, prescribing over telemedicine has seen considerable developments in policy with the DEA’s final rule on buprenorphine prescribing and their proposed rule for special registrations. At this point, research has shown that prescribing via telemedicine visits can increase access to specific treatments and encourage patient retention: evidence is never definitive, but results show telemedicine should be considered an effective tool in treating patients, especially for substance use disorders. Changes in prescribing policy on the federal and state levels by regulators and lawmakers will likely affect interstate licensure requirements, as well.
Recommendations for Enhancing Telemedicine Accessibility and Effectiveness
Considering these three areas of key concern in telemedicine policy, we provide our recommendations to stakeholders to ensure telemedicine can continue as a sustainable mode of healthcare delivery for patients.
- Simplifying and Streamlining Policies
- Lawmakers can focus on simplifying policies to reduce administrative burdens, especially for small practices.
- Clinicians may lack the resources to navigate complex licensure and compliance requirements (such challenges lead to reduced telemedicine offerings for vulnerable patients).
- Privacy and Security
- Lawmakers and regulators should refine existing privacy and security protocols to protect patient information in telemedicine contexts.
- Clinician practices should adopt advanced privacy and security technologies to safeguard patient data.
- Facilitation of Interstate Telemedicine Practice
- Stakeholders have already shown a trend of joining and improving interstate compacts to streamline licensure processes.
- Clarification of Prescribing Regulation
- Regulators can continue to provide more consistent guidelines for prescribing medications via telemedicine.
- Lawmakers and regulators should consider the vast amount of telemedicine research and data in their deliberations.
Conclusion
We briefly covered three key legal and regulatory challenges facing telemedicine in the U.S. today and provided recommendations for lawmakers and regulators to improve the telemedicine policy landscape. Healthcare cannot thrive amid prolonged policy uncertainty in telemedicine.
We encourage policymakers, clinicians, and technology developers to collaborate in implementing these recommendations to foster a more accessible and sustainable telemedicine landscape. Clinicians can prepare for the evolving policy landscape by joining interstate compacts, advocating for policy changes, and maintaining compliance with privacy and security protocols.
Author: Julia Ivanova, PhD, MA – Doxy.me